Functional genomics is a gene testing modality with enormous value that many are completely unaware of. Bob Miller1 is a certified traditional naturopath specializing in genetic-specific nutrition. He’s the founder of the NutriGenetic Research Institute,2 devoted to testing and helping people understand the results of their functional genetic testing and how to apply it to improve their health.
“As a traditional naturopath, we’re not licensed medical doctors, so we don’t diagnose, treat or prescribe,” Miller explains. “We look at the functional approach of, ‘How is the terrain off in the body?’ … [W]hen the body is toxic or inflamed, that’s when pathogens have a better opportunity to thrive.
Many years ago, I learned about how homocysteine has pathways that clear it that may be impaired by genetic variants. I became very fascinated by it. I started looking at the enzymes that clear it, and then the genetics behind it.
My whole naturopathic and holistic practice is [now] dedicated to helping clients measure their functional genomics, which is quite a bit different than traditional genetics that looks for disease patterns, and trying to find out how we can make interventions to bring the body back into balance …
Our goal is to be able to make a contribution to functional practitioners, so they can do their job a lot better and improve the lives of those who are suffering with some of those things that nobody can seem to figure out …
To sum up what we’re finding is that those with genetic weakness in detox pathways are exposed to environmental factors we weren’t dealing with 50 to 75 years ago; their ability to detox is overwhelmed. I think this is a whole new paradigm that we have to look at in wellness.
Those who don’t have a specific disease, so to speak, but are just totally overwhelmed by all of the epigenetic factors, such as pesticides, electromagnetic fields (EMFs) … excess iron … plastics … mold … [and] sometimes even oversupplementation with things like folate and glutamine … that no matter what they try, it doesn’t work …
That’s why we need to move to personalized care, based upon the individual. Fortunately, we now have tools to do that.”
What Is Functional Genetics?
Certain genes are known to predispose you to, or raise your risk of, certain diseases. That’s not what we’re talking about here. Functional genetics looks at the single nucleotide polymorphisms (SNPs, pronounced “snips”) of genes related to function.
You’ve probably seen representations of the DNA ladder. On the end of each rung is a molecule from each of your parents. These molecules can either make your DNA optimal or, if you have a SNP, meaning a defect, that gene will not work at optimal efficiency. Miller explains:
“To make this simple, we eat fats, carbohydrates and proteins. We drink water, breathe air and are exposed to sunlight. What an absolute miracle it is that all of that turns into us: our blood, our skin, our nails, our organs and our thought processes. All of that is one enzymatic process after another.
So, an enzyme takes substance A; pulls in what we call cofactors and makes substance B. That continually happens throughout your body — one process after another. It’s your genetic makeup that [provides] the instructions on how to make these enzymes.
When we have genetic variants, SNPs, on the genes, sometimes those enzymes either aren’t as effective … or might be upregulated or downregulated. Therefore, that substance A to substance B [conversion] may not occur as it should.
Now, people get all excited about whether they have genetic variants or not, but there’s something else just as important. That’s the cofactor. Remember, substance A plus cofactors turns into substance B. You could have absolutely perfect genetics, that enzyme is made perfectly, but if you’re missing the cofactors, that A to B [conversion] is not going to work …
Where people really get hit hard is when they’ve got genetic weakness and cofactor weakness. Then there’s a third piece. Sometimes there are things that interfere. For example, lead, mercury and other things may suppress that enzymatic function …
Now, interestingly, we have all kinds of backups. One pathway may not be working, but another one might kick in. But what we’re observing … is that those who are struggling usually have multiple pathways blocked. Plus, they get multiple epigenetic exposures … When you get those epigenetic and genetic factors going together, that’s when things really start going awry.”
The Relationship Between mTOR Pathway and Autophagy
Autophagy means “self-eating” and refers to your body’s process of eliminating damaged and defective cellular parts that are targeted for lysosome, which then digests them. The mammalian target of rapamycin (mTOR) is a molecular signaling pathway responsible for either growth or repair, depending on whether it is stimulated or inhibited.
I’ve often stated that to upregulate maintenance and repair (which will boost longevity and reduce your risk for cancer), you need to suppress the mTOR pathway. One of the most efficient ways to do this is to limit your protein intake, but it’s not the only way. Autophagy and mTOR are two processes that work together, but are inverse to each other. Miller likens mTOR to a construction crew, whereas autophagy refers to the cleanup crew.
“One of the ways you can tell if your autophagy is not working is when you get those age spots, sun spots, liver spots, whatever you’d like to call them,” Miller says. “That’s when the old cell is not cleared away and it becomes oxidized, it becomes senescent. It actually becomes a free radical-giving reactive oxygen species.
Now, we need a balance between [mTOR and autophagy]. We need a time to build and we need a time to clean. One of the things our research institute [found] in some of our studies on those with chronic Lyme disease [is] that we are being exposed to more epigenetic environmental factors that stimulate mTOR … ”
Factors That Activate mTOR Versus Those That Support Autophagy
Examples of environmental factors that activate mTOR include:
Xenoestrogens (chemicals in plastic) | |
Excess protein | |
Excess folic acid, folate or methyl folate | |
Excess glutamate | Amino acids such as leucine, isoleucine and valine |
When mTOR is activated, it inhibits autophagy and, according to Miller, many of the health challenges people face these days appear to be related to excess mTOR activation.
This is also one way by which a cyclical ketogenic diet helps improve your health, as it inhibits mTOR and activates autophagy. When mTOR is chronically activated, it will not only inhibit autophagy but also impair apoptosis (cell death), and if that’s impaired, your risk for cancer will significantly increase as well.
“We have identified the genes that are involved with autophagy,” Miller says. “They’re called Unc-51 like autophagy activating kinase 1 (ULK1), serine/threonine-protein kinase (ULK2), 5’ AMP-activated protein kinase (AMPK) and AuTophaGy related 1 (ATG1).
Those all stimulate autophagy. We’re finding that when people have a lot of genetic variants, especially when they inherit it from both parents, this is where their autophagy’s weakened. They’re 45 years old and covered with age spots. They can’t detox.
Ketogenic diet, intermittent fasting and nutrients [such as] lithium and berberine support autophagy. Resveratrol and curcumin slow down mTOR.
When you put the three together — the caloric restriction mimetics (CRM) [editor’s note: supplements that mimic the antiaging effects of calorie restriction] … along with the keto diet, along with some form of intermittent fasting — you’re able to bring balance to mTOR and autophagy.”
If Ketogenic Diet or Intermittent Fasting Fails for You, This Could Be Why
While intermittent fasting is an excellent strategy for a majority of people, it doesn’t work as expected for everyone. As explained by Miller, members of his research team have discovered having a functional heme pathway is extremely important when you’re on a ketogenic diet and/or intermittently fasting.
Heme protein is created through an eight-step process beginning with succinyl coenzyme A (succinyl CoA), glycine and amino acids. Heme protein in turn is a component of hemoglobin, but it’s also involved in the making of nitric oxide, catalase, superoxide dismutase (SOD) and sulfite oxidase (SUOX), which is your sulfide to sulfate conversion.
“It’s involved in so many processes that I didn’t even realize until we started to research,” Miller says. “This [heme] pathway may be impaired by … glyphosate [which impacts glycine] … lead … and genetic variants in the heme pathway.
If any of those happen, you don’t make adequate heme, so you’re going to be a very poor detoxer. Now, what’s interesting … [is that] if porphyrins [glycoproteins responsible for pore formation in cell membranes] are not transferred one to another, they will block the gamma-aminobutyric acid (GABA) receptor sites. GABA is the ‘Don’t worry. Be happy. Sleep. Relax’ [neurotransmitter]. Clearly, there are problems with anxiety in the world today.
If this heme pathway gets disturbed, people oftentimes crave carbohydrates. If they try to go keto, it doesn’t work. If they try to do intermittent fasting, it doesn’t work … It’s a small amount of people, but for some individuals who just crave carbohydrates, they’ll get hangry if they don’t have their carbohydrates. They’re actually feeding that heme pathway.
If someone’s ever tried keto and is like, ‘This just does not work for me,’ there’s a potential that the heme pathway could be impaired. You have to keep those carbohydrates coming in on a regular basis to feed it, or else you feel horrible. I remember in the past people telling me, ‘Whenever I try to eat healthy, I feel horrible. When I eat junk, I feel better.’
I used to think, ‘Yeah. I’m not sure I buy that.’ But now that you understand this heme pathway and how carbohydrates and simple sugars can feed it, it starts to make sense that that is a potential scenario for some people.”
Even if You’re Anemic, You May Be Overabsorbing Iron
As mentioned earlier, iron stimulates mTOR. Clearly, iron is crucial for optimal health. Without sufficient amounts of iron, you cannot make sufficient amounts of hemoglobin, which carries oxygen through your body. However, in excess, iron is incredibly destructive.
“Here’s one of the interesting things we found through our research. There are many people who have genetic predisposition to overabsorbing iron, yet they’re told all their life they’re anemic. It just seems like such a dichotomy; how can you be anemic if you’re overabsorbing iron?
One of the things that we … find in many who are struggling and can’t get answers anywhere else is that they overabsorb iron. There’s an enzyme called ferroportin, [which] is what takes iron out of the cells. SNPs there, or genetic defects, inhibit the removal of the iron. Through something called the Fenton reaction … iron may combine with hydrogen peroxide to make hydroxyl radicals.
This can then go on to make another nasty free radical called peroxynitrite. Consequently, the person is anemic because they are measuring what’s in the blood, but the iron can be in excess and inside the cells, causing massive inflammation.
As that iron bangs around inside the cell, it creates fatigue, because the mitochondria are having a hard time making energy. These are the people who if someone gives them iron, many times, they feel considerably worse, because they’ve just fed the fire.
In our consulting, one of the things we probably do the most is identifying the Fenton reaction going on and taking remedial action to, for example, help turn the hydrogen peroxide into water through an enzyme called catalase; supporting enzymes and antioxidants called glutathione and thioredoxin that turn the hydrogen peroxide into water, [and] using homeopathics to make the iron behave itself.”
Hydrogen water can be helpful here, Miller notes, because it helps decrease the excess hydroxyl radicals. “Quite simply, H2O2 plus iron equals hydroxyl free radical (OH-), which is one of the most highly reactive and damaging free radicals,” Miller explains.
I’ve previously interviewed Tyler LeBaron, one of the leading experts on molecular hydrogen, and he believes the benefits may be related more to the upregulation of antioxidant pathways, such as the nuclear factor erythroid 2-related factor 2 (Nrf2). Either way, whatever the mechanism, it seems clear hydrogen water has the ability to neutralize free radicals.
Situations in Which NAC or Methyl Folate May Backfire
I’ve previously written about the benefits of N-acetyl cysteine (NAC), the rate-limiting factor for glutathione, which is a master antioxidant made by your body. However, in order for this to work, you must have the required enzymes. What’s more, if you have an iron problem, the cysteine you take can combine with the iron to create hydroxyl radicals — essentially worsening your situation.
“It goes back to the fact that we’ve got to get away from the cookie cutter, ‘Oh, you’re inflamed. Take NAC.’ NAC can be the perfect thing for you, or it can make you worse, depending on your genomic make up,” Miller says.
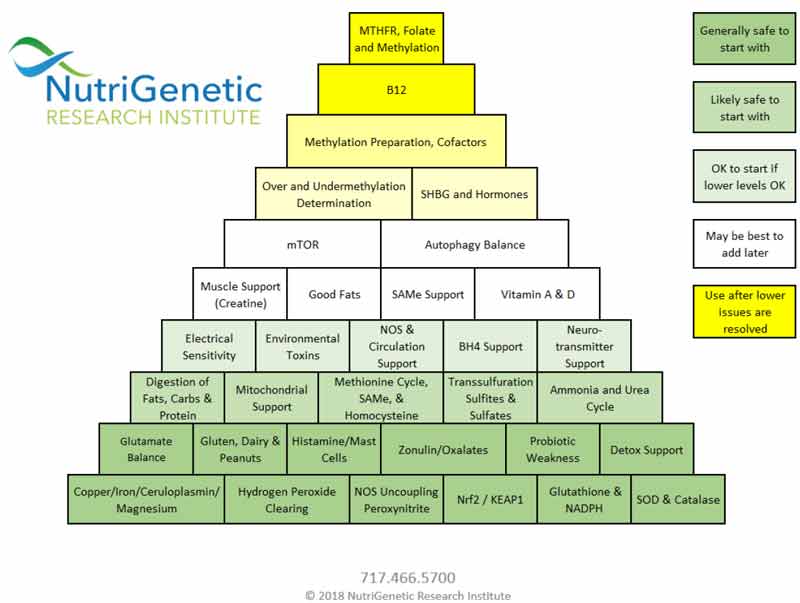
Miller has developed a hierarchical pyramid of different variables and his approach to treating them. Interestingly, many who superficially look at functional genomics think that the methylation defect is one of the most important. It is important, but according to Miller there are many others that supersede it in terms of importance.
“[Methylation] is about how we take folic acid or folate from our diet and turn it into methyl folate, which is a very important molecule. For a woman who’s pregnant, you’ve got to have it for a good pregnancy. We’re not saying it’s not a good thing … Now, one of the interesting things about methyl folate is you need it for pregnancy because it supports mTOR.
If someone’s already in mTOR dominance and they take methyl folate, they’re going to get more anxious and more inflamed. I’ve talked to so many people who’ve said, ‘Oh, yeah. I have MTHFR. Somebody put me on methyl B12, methyl folate. I felt great for two weeks, and then I crashed.’
The reason they may have crashed is because they started to stimulate mTOR, weakening their autophagy even more, driving more inflammation … As we dug deeper, we realized that methyl folate is important, but it has to be done at the right time. That’s why I developed my pyramid.
At the very bottom we have things we have to address first, such as, is iron becoming a free radical? Is hydrogen peroxide not being cleared? Is there nitric oxide synthase (NOS) uncoupling? — where rather than making nitric oxide, we make more peroxynitrite.
And then we look at how we’re making antioxidants. How’s our glutathione pathways? How’s our superoxide dismutase? How are we making NADPH? … For the most part, I believe that when people are massively inflamed, you need to address that first.
If someone is massively inflamed, if their iron is creating hydroxyl radicals, if they have weakness in their antioxidants … and you throw methyl folate in there … there’s a very good chance it will make the situation worse.
By and large, if someone’s massively inflamed, I’d like to think about methyl folate six to eight months down the road, two to three days a week. We tend to think, ‘If a little’s good for us, a lot must be good for us.’ I’m now thinking need to be pulsing things.”
I totally agree pulsing is a key component that should not be overlooked, whether you’re taking supplements, fasting or doing a ketogenic diet. It’s important to go through cycles of buildup and tear-down.
For example, during a partial fast, you’re stimulating autophagy through caloric restriction. At that time, you would not want to take anything that stimulates mTOR (such as methyl folate or any of the other items listed above), as by stimulating mTOR you effectively interrupt the autophagy process.
Mast Cells Could Be Wreaking Havoc With Your Health
Glutathione rapidly loses electrons, making it useless unless recharged by nicotinamide adenine dinucleotide phosphate hydrogen (NADPH). As explained by Miller, the “NADPH steal,” a term he coined, may also be at play in many of the health issues people face today.
It’s becoming more widely known that you can have excess mast cells. Miller estimates about 80 percent of his clients have excess mast cell activation triggering histamine reactions. One of the signs of this is redness of the face due to heat intolerance. Sensitivity to touch is another, as are frequent, red, raised rashes.
Mast cells are white blood cells that come to the rescue when there’s a pathogen or a foreign invader that needs to be eliminated. While overfiring mast cells can cause problems, they’re not inherently bad, and strategies that inhibit them can backfire. Instead, Miller recommends determining why your mast cells are overactive.
His team presented research at the International Lyme and Associated Diseases Society’s 19th Annual Conference in November last year, identifying epigenetic factors that stimulate mast cells. He explains the relationships between mast cells, NADPH, NOX and glutathione:
“In simple terms, glutathione … has one chance to give a free radical an electron. Once it does that, it becomes oxidized. Then we need to donate that electron back. There’s this substance called NADPH that donates that electron back.3 It takes that oxidized glutathione and turns it back into reduced. That’s a good thing.
Now, NADPH has a dual role. There’s also an enzyme called NOX (NADPH oxidase). Its only purpose is to take this NADPH and turn it into a free radical … Now, they’ve done studies on animals. When they knock out that NOX enzyme, the animal dies from infection because it doesn’t have the ability to kill the pathogen.
Again, NOX and free radicals are not bad. But there are multiple factors that are now overstimulating NOX. One of them is sulfite. Sulfite needs to turn into sulfates. If we have deficiency of heme, we may not turn sulfites in sulfates … If sulfites don’t turn into sulfates, the sulfites may tell the NOX enzyme, ‘You need to make inflammation.’
Dopamine stimulates it [NOX], so stress will cause it. Glutamate stimulates it. Iron stimulates the NOX enzyme, and so does excessive mTOR … The NADPH steal is when NADPH gets stolen away from recycling glutathione, recycling thriodoxine, making nitric oxide, and potentially making excess mast cells.
There are a lot of people struggling with excess mast cells firing. They’re really sick. They don’t know what to do … Mold will also stimulate mast cells …
To sum it up, NADPH is critical for recycling your antioxidants. I believe the nicotinamide adenine dinucleotide (NAD+) and the NADPH are some of the most important things we can have adequate levels of for longevity and good health. We’re using up a lot of it because we’re exposed to so many toxic substances. Then, if another set of substances are stealing it to stimulate NOX to make mast cells, then we’ve just doubled the problem.”
Molecular hydrogen serves a role here as well, as studies have shown molecular hydrogen is an effective inhibitor of NOX,4 and can increase your concentration of NADPH. Curcumin also inhibits NOX, as does luteolin, apigenin and olive leaf. Aldosterone, on the other hand, stimulates NOX, Miller says.
More Information
This interview is quite loaded with information, not all of which has been covered in this article. For even more side notes and fascinating tangents, I recommend listening to the interview in its entirety.
Health practitioners interested in learning more about functional genomic analysis and how to apply it in your own practice, see the NutriGenetic Research Institute’s website, where you can sign up for their 30-hour, 14-module online certification course to become a nutritional genetic consultant.
Webinars for health practitioners are held every other Thursday. They also hold an annual conference in Hershey, Pennsylvania. The next one is scheduled for November 2019. In September, they’re also holding a seminar on environmental toxicity, detoxification and methylation mapping.
Patients interested in more information are directed to the yourgenomicresource.com which includes a listing of doctors who have completed the training and are qualified to provide nutritional guidance based on your SNPs. Up until last year, Miller could guide patients based on the genetic data provided by companies such as 23andMe. Now, he has developed his own DNA testing, which is capable of identifying some 300,000 SNPs.
Importantly, NutriGenetic Research Institute will never sell your private DNA or health data to anyone, which is one of the reasons why 23andMe is so inexpensive — they make their money by selling your DNA results to drug companies.
“I have pledged to everyone in writing that this data will never be sold to anyone. The other thing people can do, if they’re still worried, you can just change your name. Just come up with a fake name. It doesn’t matter. We don’t care. You just have to remember what it is,” Miller says.
“The [DNA] data from Brooks at Rutgers gets loaded into my software, which is in Chambersburg, Pennsylvania — a huge database. Then it crunches the data and gives a report, including the pyramid …
If you’re sick, you’ve been everywhere and you’re not getting better, this is certainly an option … Our whole goal is to help people get well. And to make a little bit of a dent in functional medicine — to help functional practitioners have tools that they can help, because functional medicine doctors see the tough cases. We want to give them some tools so that they can do a better job …
One of my favorite sayings is, ‘Genetics is never a diagnosis, but it tells you where to start looking.’ It’s like shining a light. ‘Think about looking here. Investigate whether this is a problem.’ Sometimes the SNPs show a problem, sometimes they don’t, but it can really give you clues to look where you may never have thought to look before.”
