In the United States, 85 percent of women will get pregnant in their lifetime (and that number is higher in other countries). While the majority of women will have vaginal births, about 32 percent will have C-sections. And the percentage of women who have C-sections continues to increase, both in the United States and around the world.
With rising C-section birth rates and mounting evidence of the benefits of exercise in the postpartum period, it’s more important than ever to recognize how instrumental you as a coach can be in helping women return to exercise safely after a C-section.
In this article, we’ll:
- Help you understand what a C-section is, and the different types of C-sections some of your postpartum clients may have had.
- Discuss the physical and mental/emotional benefits of exercise in the postpartum period.
- Address the problems with the typical “six weeks” advice for returning to exercise after a C-section.
- Talk about why postpartum rest and recovery are vital and why return to exercise cannot be rushed.
- Show you, step by step, how you can help your clients safely return to exercise after a C-section birth.
What Is a C-Section?
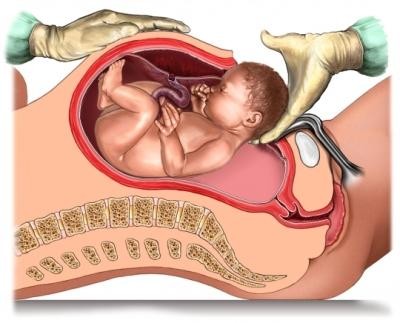 A Caesarean — or C-section — is the delivery of a baby through a surgical incision in the abdomen and uterus. It involves the use of epidural or spinal anesthesia, and in some critical cases, general anesthetic.
A Caesarean — or C-section — is the delivery of a baby through a surgical incision in the abdomen and uterus. It involves the use of epidural or spinal anesthesia, and in some critical cases, general anesthetic.
Planned and Unplanned C-Sections
A C-section may be planned and scheduled in advance, or it can be unplanned such as in vaginal births where circumstances require a change of plans, or in an unforeseen emergency situation. However, not every unplanned C-section is an emergency procedure.
Some women experience distress and trauma after an unplanned C-section birth. When working with postpartum clients who had an unplanned C-section, keep in mind that while some women may feel an immense sense of relief and joy that the baby was born safely, they may still experience feelings of failure and disappointment about the change of plans.
Knowing if your client had a planned or unplanned C-section will help you better understand your client, her views about her body, and her sense of autonomy.
Recovery From a C-Section
In the U.S., women who’ve had a C-section will typically stay in the hospital for two to three days. In other countries, they may stay up to five days.
Your client’s recovery from a C-section depends on factors including:
- Birth circumstances (elective C-sections are often easier to recover from)
- Her previous level of fitness
- Care taken during recovery
- Support at home (and the presence of other children to look after)
- Timeliness of pain medication
Her experience of pain may also vary. While some women experience severe pain and discomfort and struggle with simple acts of self-care, others may only experience mild discomfort with exertion. Pain may be stabbing and intermittent or a dull ache. Generally, sudden movements can cause sharp pains.
Pain typically decreases over the first five days, and most women no longer need pain relief medication by seven to 10 days after birth.
Benefits of Exercise in the Postpartum Period
There is far more research available on exercise in pregnancy than in the postnatal period, and most of the research related to exercise in the postnatal period is on its effects on mental health. There really isn’t much dedicated to the other aspects of physical health.
However, here are some evidence-backed benefits of postnatal exercise that you can mention to your clients:
Physical
- Enhances cardiovascular health through improved glucose tolerance, lipid profiles, and vascular function.
- Improves aerobic function (VO2max)
- May reduce body fat and improve basal metabolic rate, especially for women who aren’t lactating.
- May improve bone mineral density or prevent lactation-related bone loss in women who are breastfeeding.
- May help children form more regular physical activity habits.
Mental and Emotional
- Has a positive effect on well-being and symptoms of depression.
- Improves mood and body image.
- Reduces rates of postnatal anxiety and depression.
- May improve the rate and severity of postpartum depression.
And of course, let’s not forget the positive benefits of exercise in general, as it:
- Protects against the development of chronic disease.
- Improves respiratory function.
- Reduces risk of coronary artery disease.
- Decreases blood triglycerides.
- Increases HDL.
- Improves insulin sensitivity.
- Reduces visceral fat.
- Decreases death rates from coronary artery disease.
- Decreases rates of cardiovascular disease, stroke, type 2 diabetes, bone fractures (due to osteoporosis), and some forms of cancer (breast/colon).
OK, it’s clear that exercise and movement in the postpartum period are beneficial… so, how soon can your client return to exercise after a C-section, and what activities are safe for her to do?
The general guidance around this, which you may have heard, says that C-section clients can return to their usual exercise habits in as little as six weeks.
Let’s take a magnifying glass to that advice and explore what’s really best for your client.
Returning to Exercise After C-Section: The “Six Weeks” Myth
For generations, women have been told that their postpartum period lasts just six weeks — from the day they give birth to the day of their six-week checkup with their doctor.
Six weeks. Let’s talk about that for a moment.
 Yes, many women usually notice a steady reduction in pain over the first few weeks postpartum, with minimal pain when performing activities of daily living by the six-week mark. And at the six-week checkup, many medical professionals advise their postpartum patients to gradually increase exercise as they are able.
Yes, many women usually notice a steady reduction in pain over the first few weeks postpartum, with minimal pain when performing activities of daily living by the six-week mark. And at the six-week checkup, many medical professionals advise their postpartum patients to gradually increase exercise as they are able.
But considering that a C-section is a major abdominal surgery that will require healing across several layers of tissue, it’s baffling that women are told it’s OK to return to normal function after only six weeks.
We consider this a “myth” for two reasons.
On one hand, advising women to do nothing until they reach the six-week mark can hinder their recovery.
As they heal, it’s actually fine for most women to move in ways that are no more strenuous than the tasks of daily living, and gentle movement can encourage healing.
On the other hand, it’s harmful to suggest that all women can be fully cleared to do any activity they want to do at just six weeks.
Musculoskeletal injuries may take between six months to a year — and that’s exactly what a C-section is.
A C-section may be common, but it’s not a gentle or minor procedure. The healing process is not complete at six weeks. In fact, a C-section scar has only 51–59 percent of its original tensile strength at six weeks post-surgery. On the surface, the C-section scar might appear healed, but the deeper layers underneath the skin still need time. The scar alone is several layers deep — tissues that aren’t visible are still recovering.
Think of surgery such as an ACL repair in the knee. Rehab for an ACL repair takes nine months to a year. The patient will work toward several milestones and have regular checkups along the way with the surgeon and the physiotherapist, and an evidence-based timeline dictates when it’s safe to return to certain activities.
(By the way, all the experts who consulted on or contributed to our Pre- and Postnatal Coaching Certification course agree this is how recovery from a C-section should be treated as well.)
However, the research available on recovery from C-section offers minimal information on how to proceed. The guidelines given for the first six weeks postpartum are based on theory rather than on hard evidence.
For instance, women are often advised not to lift after giving birth based on the idea that lifting weights will increase intra-abdominal pressure and place too much pressure on the healing abdominal muscles and pelvic floor. But researchers have found that for some women the intra-abdominal pressure created when lifting 35 pounds (16 kg) from a counter or 40 pounds (18 kg) from the table or the floor is less than the pressure created when moving from supine to upright position or when walking up a flight of stairs.
They also found that for many women getting up from a chair increases intra-abdominal pressure more than many other activities that women are routinely advised to avoid, such as crunches and lifting as little as 13 pounds from the floor.
These findings suggest that some activities women might do in the gym could actually be less taxing on the abdominal muscles and pelvic floor than activities they are likely already doing as part of everyday life, such as lifting their kids, carrying groceries, or performing physical tasks around the house.
As you can see, many postpartum activity recommendations may be confusing, conflicting, or downright difficult to follow for some women — especially those who may be caring for other children in addition to a newborn.
With all that said, clients may want to return to exercise in some way — and turn to you for help. Here’s how you can support those clients.
1. Recognize That Every Person Is Different
If you’ve worked with postpartum clients for a while, you may notice that recovery after C-section is highly variable.
Here are some things to keep in mind.
How Is She Healing and Feeling Physically?
Some of the more common issues that women may face after C-section include pain, reduced mobility, problems with the abdominal wound (e.g., infection), vaginal bleeding, and incontinence. Some women will heal rather quickly, and some may take much longer to recover, particularly if they had a traumatic birth.
Your client should have a postnatal check with her doctor to make sure she’s healing well and has clearance for exercise. (If any of these issues crop up during the postnatal period, you should always refer her back to her doctor.)
What Is Her Exercise History?
How active your client was prior to pregnancy and during pregnancy can have an impact on her ability to return to exercise.
What Were Her Pregnancy and Birth Experience Like?
Things like whether she had pain or incontinence during her pregnancy, how long her delivery lasted, whether she had any injuries, and whether she’s had multiple births may all make a difference to her body’s ability to return to exercise.
 All that said, there are some general guidelines to consider. In our progressive 42-week postpartum training program (which you’ll learn more about in a moment), we recommend that a client who had a vaginal birth follow a six-week rehab and retraining phase starting within days of giving birth, before entering the next two phases of our postnatal training plan.
All that said, there are some general guidelines to consider. In our progressive 42-week postpartum training program (which you’ll learn more about in a moment), we recommend that a client who had a vaginal birth follow a six-week rehab and retraining phase starting within days of giving birth, before entering the next two phases of our postnatal training plan.
For a client who had a C-section, however, we recommend pushing the timeline back an extra two weeks based on how the scar is healing; perhaps starting about two weeks after the C-section. If the scar isn’t healing well, there are other complications, or your client feels she needs more time, we recommend pushing that start day back even further.
In a moment, we’ll show you how to assess your client — but for now, the most important takeaway is that there are no hard and fast rules.
Every person is different, and every woman’s experience is unique.
2. Consider Her Psychological Health
There’s a reason that postpartum psychology is the first chapter after the birth process in our Pre- and Postnatal Coach certification textbook.
It’s normal for a new mother to experience weepiness and irritability, also known as “baby blues” in the first days or weeks after giving birth. In fact, it’s estimated that 40–80 percent of new mothers experience the baby blues due to significant changes in their hormones — primarily a large drop in estrogen and progesterone. In most cases, the baby blues subside, although the impact of hormonal changes may persist.
Some women experience low moods for a month or more after birth. This is a symptom of postnatal or postpartum depression (PND or PPD). Women with postpartum depression may also experience poor sleep, low energy, decreased pleasure, hopelessness, constant negative feelings and thoughts, and an inability to cope.
According to the Center for Disease Control and Prevention, 11.5 percent, or approximately one in nine women experience postpartum depression in the U.S.
In cases of traumatic birth, women may develop postpartum post-traumatic stress disorder or P-PTSD, which includes flashbacks and nightmares about the birth, physical reactions like heart palpitations, nausea, faintness when seeing a hospital or hearing about birth.
Always be sensitive around your clients’ birth experiences. Be supportive and refer on as needed.
If a client is experiencing postpartum depression or postpartum post-traumatic stress disorder, advise her to seek help from her general practitioner and get a referral to a qualified mental health professional.
When Your Client’s Birth Experience Didn’t Go As Planned
When a woman’s birth experience is different than what she expected or imagined, it can deeply impact her psyche and emotions, the way she views herself and her body, and her sense of self — sometimes for life. Some examples of birth experiences that can cause a woman to struggle:
- Traumatic births that pose a danger to the mother or the baby or that end in emergency procedures or in the loss of the baby
- Labor that lasts many long hours or extends through days
- Insensitivity from medical professionals or accompanying family
- Pressure to make difficult decisions
- Unforeseen complications
- Unexpected procedures
- Painful injuries
Any of these experiences can contribute to a woman’s feelings of being betrayed by her body — even if her baby is safe, healthy, and thriving.
A woman whose birth experience differed from what she desired or expected may need a grieving period because it’s a loss of sorts to her.
This may sound drastic, especially if you haven’t experienced childbirth or if you are happy with your own childbirth experience.
We cover a lot more on these topics here and here.
3. Understand Common Concerns and Roadblocks of Postpartum Clients
Gaining a real understanding of these will go a long way in helping your client.
Stress and Lack of Sleep
It may not be possible for your client to sleep well every night, but any small amount of rest she can get is likely to improve her mood, energy, metabolism, and hormones, decrease her stress, support her immune system response, and assist with tissue healing and recovery.
Stress and lack of sleep can:
- Affect circulation, which can increase muscle and nerve sensitivity and tenderness and result in more aches and pains).
- Cause the body to produce more cortisol, which can lead to unwanted weight gain.
- Decrease blood flow to the digestive system, which can lead to stomach sensitivity
- Alter the testosterone and estrogen, which can lead to a lower sex drive.
- Negatively affect mood and the ability to cope.
It’s easy to see how stress can significantly affect recovery and healing — and even more so, considering the additional tissue healing required after a C-section.
Abdominal Pain and Scar Tissue Stiffness
Remind your clients to be gentle with their body in the weeks and months following childbirth. Abdominal pain and scar tissue stiffness are both common after C-section.
Other common concerns and roadblocks for both vaginal and C-section postpartum clients include low back pain, pelvic girdle pain, diastasis recti, pelvic organ prolapse, and incontinence.
4. Assess Your Client
Assess your postpartum client before she returns to any type of exercise that’s more strenuous than the tasks of daily living. So, if you’re using our 42-week postpartum program as a roadmap for training your postpartum client, you would assess after the six-week Rehab and Retraining phase, before she starts the Return to Exercise Phase.
To start, confirm that at her six-week checkup, your postpartum client received clearance from her doctor to return to exercise. If she was cleared to return to exercise, you’ll take her through a screening process that includes a questionnaire and a movement screen, just as you would with any other client. However, your screening process should be specifically designed for postpartum women.
PPAR-Q
The Postnatal Physical Activity Readiness Questionnaire (PPAR-Q) will not only guide your exercise programming considerations, but it will also help you determine when to refer a client to another professional.
 Ideally, you will send the PPAR-Q to your client electronically before your initial appointment, in order to flag any potential issues ahead of time. The questionnaire will help you screen for any potential contraindications to exercise, as well as identify whether a client would benefit from a multidisciplinary approach to her rehabilitation. It’s better to know about this in advance to save you both time and get her the help that she needs even sooner.
Ideally, you will send the PPAR-Q to your client electronically before your initial appointment, in order to flag any potential issues ahead of time. The questionnaire will help you screen for any potential contraindications to exercise, as well as identify whether a client would benefit from a multidisciplinary approach to her rehabilitation. It’s better to know about this in advance to save you both time and get her the help that she needs even sooner.
Along with general information, such as name, contact details, and emergency contact, you should obtain information about your client’s delivery date and type (vaginal or C-section), number of pregnancies, the outcome of her six-week check-up, and her breastfeeding status.
Collecting details about any complications of the pregnancy and postpartum period, such as illness and whether she has visited healthcare practitioners (e.g., doctors or physiotherapists, chiropractors, or acupuncturists), will also give you valuable information for your programming. Your PPAR-Q should also include questions about scar tissue healing, pain, and lochia (the vaginal discharge from the uterus after childbirth, which contains blood, mucus, and uterine tissue).
Visual and Physical Movement Assessments
Performing a movement screen will help you identify potential postural issues at the outset so that you can program some remedial work to correct any imbalances that might be relevant. You might even be able to identify these postural compensations the moment your client walks through the door.
We think that the following are important to assess in the postpartum population.
Standing Posture
When looking at standing posture, try not to draw any initial conclusions from what you see — just observe and document. Remember that everyone will have asymmetries, leg length discrepancies, or little postural quirks, many of which are not causing them pain or dysfunction.
Breathing Patterns
Assessing breathing patterns is very important for everyone but in particular the postpartum clients, who often adopt poor strategies when recovering from pregnancy. Observe how your client breathes throughout the screening process. How does she breathe when sitting upright and when lying supine, where gravity changes the pressures in the abdomen?
A breathing pattern disorder often shows up as an upper-chest breathing pattern and hyperventilation and may be accompanied by symptoms like mood changes, anxiety, increased pain sensitivity, and neck/shoulder pain. Some clients may avoid taking big abdominal breaths after a C-section because of pain or because they’re concerned about their scar. It is important to encourage relaxation of the abdominal wall, allowing that distension on the inhale.
Diastasis Recti
You may already be familiar with diastasis recti, which is when the abdomen expands in pregnancy and the linea alba stretches, increasing the distance between the rectus abdominis muscles. This is considered a normal part of growing a baby.
Research has shown that in the final trimester of pregnancy pretty much every woman will have a diastasis recti of more than 16 millimeters (more than two-thirds of an inch, or about two finger breadths).1 Nearly two-thirds (60 percent) of women still have a separation of two fingerbreadths or greater at six weeks postpartum, and that separation can remain present in close to half (45.4 percent) of women at six months postpartum, and in about one-third of women (32.6 percent) at one year postpartum.2
As a pre- and postnatal coach, it’s important for you to know how to assess the extent of the inter-recti gap, when to refer your client to a healthcare practitioner, and how to monitor your client’s abdominal wall during exercise. Learn more about diastasis recti in this article.
C-Section Scar
In addition to assessing your client’s movement, make sure you visually assess her scar and how the scar site feels for her as she moves.
The scar should be well healed, with no fluid leaking. The skin around the scar should not look red or inflamed. If you or your client have any concerns, refer her back to her health care practitioner.
Remember: your screening process should be based on your scope of practice and your expertise. Our Pre- and Postnatal Coach certification course discusses screening and assessments in depth. If it’s within your scope of practice, it may be appropriate for you to palpate (touch) the scar tissue, feeling for heat, tenderness, and thickness.
5. Adjust Your Client’s Program Based on Her Recovery Experience
We break down postpartum recovery into three main phases:
- Rest, Rehabilitation, and Recovery (weeks 0–6)
- Returning to Exercise (weeks 7–18)
- Bulletproof Your Body (weeks 19–42)
However, every postpartum client’s recovery timeline may vary slightly. Use our phases as a roadmap, but always adjust your client’s program based on her recovery experience and timeline.
Rest, Rehab and Recovery (Weeks 0–6)
You probably won’t be working with your client in person during the first six weeks after she has given birth. However, she may consult you for some advice or support. It’s reasonable to expect that by the six-week mark, symptoms of pain or incontinence related to pregnancy and delivery should have settled. But remember that with a C-section client, this time frame should be pushed back by about two more weeks to allow the C-section scar to close.
Goals of Exercise During the First Six Weeks Postpartum
- Practice contracting and relaxing the pelvic floor muscles (ideally, your client will have seen a pelvic health physiotherapist for advice on how her pelvic floor muscles are functioning).
- Relieve any aches and pains in the spine.
- Work on optimal breathing pattern.
- Begin a gentle walking routine.
- Work on alignment and proprioception (awareness of the body in space).
Rushing through this phase won’t speed up recovery and could lead to more dysfunction and ultimately, a slower return to exercise or sports.
Exercise Options During This Phase
As long as your client’s doctor gave her clearance — and if your client feels up to it — she can do some breathing exercises and gentle movements during the first six weeks postpartum that are no more taxing than her activities of daily living.
Here are some things you may suggest your client try:
Core-Pelvic Floor Connection Breath
This can help with regaining body awareness and better muscle function. Learn more about the connection breath in this article.
Walking
 We recommend starting with no more than a walk around the block (or about 10 minutes) on her first outing. Whether they had a C-section or vaginal birth, many women feel quite sore in the first week and a half or so after birth. Long periods of standing and walking may make that soreness worse.
We recommend starting with no more than a walk around the block (or about 10 minutes) on her first outing. Whether they had a C-section or vaginal birth, many women feel quite sore in the first week and a half or so after birth. Long periods of standing and walking may make that soreness worse.
If your client feels no heaviness or pain after her first short walk, she can try to go a little farther or add a few minutes the next time. As she adds time or distance to her walks, taking two short walks per day might feel better than a single, longer walk. And if she can go without the stroller/pram on at least some of her walks, she can work on her arm swing and trunk rotation.
Basic Stretching and Mobility
In the early postpartum days, some gentle movement can be quite soothing for your client’s sore muscles and aching joints. She may start with more supportive movements, such as pelvic tilts and knee rolls in supine-lying position with knees bent, and build from there. These gentle exercises will also encourage some low-level abdominal muscle activation.
She can also try some neck, shoulders and upper back mobility work, such as basic neck stretches, shoulder girdle circles, and thoracic rotations.
Returning to Exercise (Weeks 7–18)
By this point, your client should have had a postnatal assessment with her general practitioner or OB-GYN and should have been cleared for exercise. If her C-section wound is closed, she can do some scar tissue massage which may help reduce adhesions and discomfort.
Goals of Exercise During Weeks 7 to 18
- Monitoring the scar tissue to make sure it’s healing as expected.
- Mobilizing the scar tissue.
- Recovering pelvic floor muscle activation and function.
- Establishing an optimal breathing pattern.
- Building some baseline strength with simple functional movements
- Improving aerobic fitness.
- Assessing and monitoring diastasis recti.
Guidelines for postnatal exercise may include a combination of aerobic exercise and strength training, along with stretching and recovery.
Your client may struggle with time constraints and fatigue, so take her time and energy into account when writing her program and be ready to modify her workouts to meet her where she is. For example, program fewer sets of each exercise so she can complete her sessions in less time, or if she’s training at home, show her how she can split her workout into multiple mini-sessions throughout the day.
Exercise Options During This Phase
Here are some options your client may try during this phase.
Breathing and Core-Pelvic Floor Connection
The breathing pattern is the foundation for everything else in postnatal exercise. In these early weeks, the focus should be on encouraging the connection between the brain and the pelvic floor muscles using the connection breath and working on increasing endurance of the pelvic floor muscles as guided by a pelvic health physiotherapist, within the client’s ability.
Encourage your client to activate her pelvic floor muscles as she performs the more challenging parts of an exercise. Generally, the challenging part of an exercise is performed on the exhale breath, and the pelvic floor muscles naturally lift during the exhale, acting in a protective fashion to support the spine, pelvis, and organs.
She likely won’t have to continue to actively contract the pelvic floor with every exercise, but early in the postnatal period it can be useful to work on this connection as the pelvic floor adjusts to a new length (i.e., without a baby sitting on top of it!).
Abdominal Wall Assessment and Strengthening
If you have been trained to assess for diastasis recti, it would be appropriate to assess this at your client’s first postnatal session. If the DRA is wide or deep, then consider referral to a pelvic health physiotherapist for management.
Many women feel that their abdominal muscles are “weaker” after C-section and some find it difficult to feel a good connection to the lower abdominal muscles. Start some gentle exercises to connect and strengthen the abdominal wall — this may include exercises in crook lying position, such as knee fall outs or leg slides, or four-point belly hugs.
Gentle Mobility Exercises
The types of movements your client was doing in the previous phase may be suitable for her warm-up.
Cardio
Your client may do some cardio at this point, but the intensity should remain low or moderate at the start of this phase. We also recommend starting with low-impact exercise to minimize strain on the pelvic floor, gradually increasing the impact as healing continues.
By 7–12 weeks postpartum, your client may be able to walk up to 45 minutes per day at an easy, restorative pace, as her energy level and schedule permits. And in weeks 13–18, if she is not experiencing pain or urinary incontinence, she can increase her time to 60 minutes per day. She may be able to ease back into some moderate-intensity and high-intensity training if she feels up to it, although we do recommend a pelvic floor assessment prior to high-impact activities.
Strength Training
She may participate in strength training two to three days per week, and we recommend staying within 2–3 sets of 8–12 reps to work at a load that elicits tissue changes and minimizes the risk of causing damage. During weeks 13–18 postpartum, she can add a 15-minute walk after her strength training workouts.
Include progressions that help her safely transition to more intense exercise. Focus on exercises that do not exacerbate diastasis recti or place excessive downward pressure on the pelvic floor.
Avoid exercises that:
- Cause pain (e.g., the low back, abdominal wall).
- Cause symptoms of incontinence.
- Result in heaviness or dragging sensation in the perineum.
- Cause a visible bulge along the linea alba.
Rest
Encourage your client to get as much rest as she can throughout the day.
Bulletproof Your Body (Weeks 19–42)
Once your client has established some baseline strength and is feeling more energized, assuming she doesn’t have any major complications or setbacks, she may be ready to do a little more. Again, postpartum recovery time frames vary, so be flexible.
Goals of Exercise During Weeks 19 to 42
- Continue maintenance pelvic floor exercises.
- Increase the strength of the abdominal wall.
- Review breathing pattern.
- Increase aerobic exercise capacity.
- Progress strength training.
- Begin sport-specific training (if appropriate).
The timeline in this phase isn’t set in stone, and sometimes weekly guidelines can put a lot of pressure on a client to progress faster than they’d like to or are able to — however, if your client is healing well and anxious to get back to exercise, this is a pretty realistic timeline that will help keep her from jumping into intense exercise too quickly.
Exercise Options During This Phase
 Your client may feel ready for higher-impact exercise or heavier weights. She may also be anxious to return to her favorite sport or physical activity. Treat returning to exercise after a C-section just as you would treat returning to any other activity — slowly progressing over time based on feedback.
Your client may feel ready for higher-impact exercise or heavier weights. She may also be anxious to return to her favorite sport or physical activity. Treat returning to exercise after a C-section just as you would treat returning to any other activity — slowly progressing over time based on feedback.
Consider the elements of the sport to which your client wishes to return. Does it require quick acceleration? Changes of direction? Hopping? Throwing? Break down the relevant movements and help her build the components she needs to return to sport with confidence.
Here are some options your client may try during this phase.
Pelvic Floor Muscle Exercises and the Core-Pelvic Floor Connection
By now, your client will be on a maintenance program of pelvic floor muscle exercises guided by her pelvic health physiotherapist, ideally. This may include performing regular sets of fast and slow contractions daily.
Ultimately, she shouldn’t be consciously focusing on her pelvic floor muscles when performing more dynamic movements. The core-pelvic floor connection should be occurring naturally by now if she has been working on it up until this point.
Cardio
In weeks 19 and beyond, your client may slowly progress toward higher-impact cardio exercise. As her energy and schedule permit, it may be OK for her to do:
- 1–2 high-intensity training (HIT) sessions per week
- 1–2 moderate-intensity cardio (MIC) sessions per week
- A walk or any other restorative activity daily
Running
If your client enjoyed running before and during pregnancy, she may be eager to start again. Encourage her to return to it gradually by increasing distance or time, and then speed, over several weeks and months. We often recommend a slow progression such as using a beginner “Couch to 5K” program and monitoring for symptoms.
Before your client returns to jogging and running, include some lower-impact exercises to master the technique and minimize any pelvic floor symptoms or pain. Exercises such as:
- High knees
- Arm swings
- Thoracic rotations
- Single-leg squat variations (which can progress to include alternating arm swings and thoracic rotations to simulate running).
Strength Training
If your client is strength training, she should perform exercises that feel comfortable and safe as she progresses toward using heavier weights and performing more complex movements. She should be pain-free and should not be leaking urine or feeling heaviness in her pelvic floor.
She can strength train two to four days per week as her energy and schedule permit, staying within 2–4 sets of 8–12 reps. She can add a 15-minute walk or HIT session after two of her strength training workouts.
Once your client has completed 42 weeks of postpartum recovery workouts, if she followed the guidelines we teach in our Pre- and Postnatal Coach certification, we feel confident that she can return to any other training or activities she enjoys, assuming she is cleared by her doctor or physiotherapist and doesn’t have symptoms of pelvic floor dysfunction.
6. Connect With Pelvic Health Physiotherapists in Your Area and Encourage Your Postpartum Clients to Work With Them
Whether your client had a C-section or vaginal birth, she will benefit from seeing a pelvic floor physiotherapist around the 6- to 8-week mark (or earlier if symptomatic) to make sure she’s healing well and her pelvic floor is functioning appropriately.
Invest some time toward building your referral network and connecting with pelvic floor physiotherapists in your area. Search any of the websites below looking for terms such as “pregnancy/postpartum,” “pelvic,” or “women’s health” under specialty or area of practice:
Want to Know More?
There is so much more to working with postpartum clients, particularly with those who have had a C-section. While this article provides an overview of some of the most important things you should know, it’s just the tip of the iceberg.
Consider this the beginning of your learning experience, not the end.
By growing your understanding of the postnatal experience, and responding to your client’s unique body, experience, needs, and goals, you can help them not only heal and recover but thrive.
If you’re a health, fitness, or nutrition professional (or you want to be)…
Learning how to coach your pre- and postnatal clients, patients, friends, or family members so that they can feel healthy and strong through pregnancy and beyond is both an art and a science.
If you’d like to learn more about both, consider enrolling in our Pre- and Postnatal Coaching Certification, which opens for enrollment VERY soon.
Our Pre- and Postnatal Coaching Certification is the most respected coaching certification in the world for working with pregnant and postpartum women
If you’re like most of the folks who enroll in our certification, you’re probably aware — maybe from personal experience — there’s a serious gap in high-quality, well-vetted, up-to-date information about helping pre- and postnatal women.
And that’s precisely why we created our Pre- & Postnatal Coaching Certification.
This certification gives health, fitness, and nutrition professionals — and aspiring professionals — the skillset, knowledge, and toolkit they need to successfully and confidently coach pregnant and postpartum women.
Our Coaching and Training Women Academy has certified thousands of professionals in 70+ countries around the world. Their results have been astonishing.
Now, we’re offering all that knowledge and training to you.
Interested? Add your name to our no-obligation pre-sale list. You’ll save up to 33% and get a chance to secure your spot before it opens to the public.
On February 11th, 2020 we’re opening enrollment to our Pre- and Postnatal Coaching Certification to a limited number of students.
To learn more, check out our pre-sale list which gives you two huge advantages:
- You’ll pay less than everyone else. The students who are most eager to level up their coaching skills are our most successful students, so we like to reward those who join the pre-sale list by offering a discount of up to 33% off the general price.
- You’ll get to enroll early. We only open enrollment twice per year, and spots always sell out FAST. By joining the pre-sale list, you have the chance to enroll 24-48 hours before the general public, increasing your chances of getting a spot.
If you’re ready to learn exactly how to keep your pre- and postnatal clients and patients safe, healthy, and strong, during and after pregnancy…
This is your chance to enroll in the world’s most respected Pre- and Postnatal Coaching Certification.