Introduction
Access to sexual and reproductive health (SRH) care in the U.S. is influenced by a variety of factors, including patients’ coverage, social determinants of health, as well as federal, state, local, and institutional level policies. We have also seen that health care providers play a large role in the care patients receive. To better understand how the provision of SRH care varies across the U.S., and how delivery of care has been influenced by changes in reproductive health policy, KFF conducted a nationally representative survey of OBGYNs across the United States. While we acknowledge that many types of clinicians are critical sources of SRH care — from midwives, to advance practice clinicians to primary care physicians— obstetrician-gynecologists (OBGYNs) comprise the largest subset of providers in this field.
This survey asked OBGYNs about a wide range of issues, including their provision of contraception, abortion, and STI care, the role of Medicaid in the delivery of SRH, screening practices for psychosocial needs, and the impact of federal and state policies on health care quality and access.
Key Findings
Contraception:
- Nearly all OBGYNs offered their patients some forms of contraceptive care, but just 18% of OBGYNs offered their patients all methods of non-permanent contraception that must be either prescribed or provided by a clinician. These methods include the pill, patch, ring, diaphragm or cervical cap, intrauterine devices (IUDs), contraceptive implants (Nexplanon), contraceptive injections (Depo-Provera) and emergency contraception (Copper IUD and Ulipristal Acetate/Ella). Those that offered all methods tended to be younger and work in large practices, with more than 10 clinicians.
- While the vast majority of OBGYNs provided both types of long-acting reversible contraception (LARCs) —IUDs (96%) and implants (84%— only four in ten of those who provided these methods offered same-day placement. This means that at the majority of OBGYN practices, patients must make more than one visit to obtain a LARC.
- Less than half of OBGYNs reported that they provided prescription forms of emergency contraception, which can prevent pregnancy after unprotected sex or in the event that a condom breaks. 45% provided the copper IUD and 42% provided Ella (the prescription “morning after pill”). Nearly four in ten reported that they do not provide either of these forms of emergency contraception.
Abortion:
- Most OBGYNs (75%) reported their practices did not provide abortions for pregnancy termination, but over one in five (23%) worked in practices that do. Abortion provision was more common among OBGYNs in urban and suburban locations compared to rural, and in the Northeast and West compared to the Midwest and South.
- The majority of OBGYNs who do not offer abortions refer their patients to other providers for this service, but just over one in ten (13%) neither provide nor refer for abortions. Among those who do not provide abortions, the most commonly cited reasons for not doing so included their practice having a policy against it (49%), saying that services are readily available elsewhere (45%) and personal opposition to the practice (31%). A higher share of OBGYNs in the Midwest and South cited legal regulations as a reason for not providing abortions, compared to those in the Northeast and West.
Other Sexual and Reproductive Health Services:
- The vast majority of OBGYNs provide onsite testing for gonorrhea and chlamydia (99%), syphilis (90%) and HIV (87%) at their practices. About half of OBGYNs said they always or often prescribe expedited partner therapy (EPT) for sex partners of patients with gonorrhea or chlamydia. Fewer than one in five (18%) prescribe pre-exposure prophylaxis (PrEP) for the prevention of HIV.
- About a quarter of OBGYNs (28%) work at practices that provide gender affirming care, including hormone therapy or gender affirming surgery. While the vast majority of OBGYNs reported they felt somewhat or very prepared to meet the SRH needs of lesbian, gay, bisexual and queer patients (88%), just over half felt the same for transgender patients (56%).
- Screening for psychosocial needs varied tremendously, with far more OBGYNs reporting they screen all patients for intimate partner violence (70%) and depression (71%) than transportation (17%) and housing (19%) needs. In the event of a positive screen, few OBGYNs said they had access to resources onsite to address these needs.
Medicaid:
- Nearly four out of five (78%) OBGYNs reported their practice accepts Medicaid. Many noted challenges associated with providing care for Medicaid patients, including difficulty finding specialists to accept referrals (73%), and being reimbursed at a lower rate than under private insurance (90%).
- A sizeable minority said they had encountered at least one Medicaid restriction regarding contraceptive care, including needing to obtain prior authorization (45%), being limited to an initial contraceptive supply of 30 days (33%), requiring “step-therapy” (15%) or being denied immediate replacement of expelled or removed LARCs (15%).
Policy Perspectives:
- Many OBGYNs are aware of the impact of out-of-pocket costs on their patients. About half of OBGYNs (53%) said the issue of affordability comes up always or often when they recommend tests or treatments to patients, and a similar share of OBGYNs (53%) said they were always or often aware of the magnitude of their patients’ out-of-pocket costs. Nearly all (92%) reported that the cost of reproductive health care poses a burden for low-income patients in their practices.
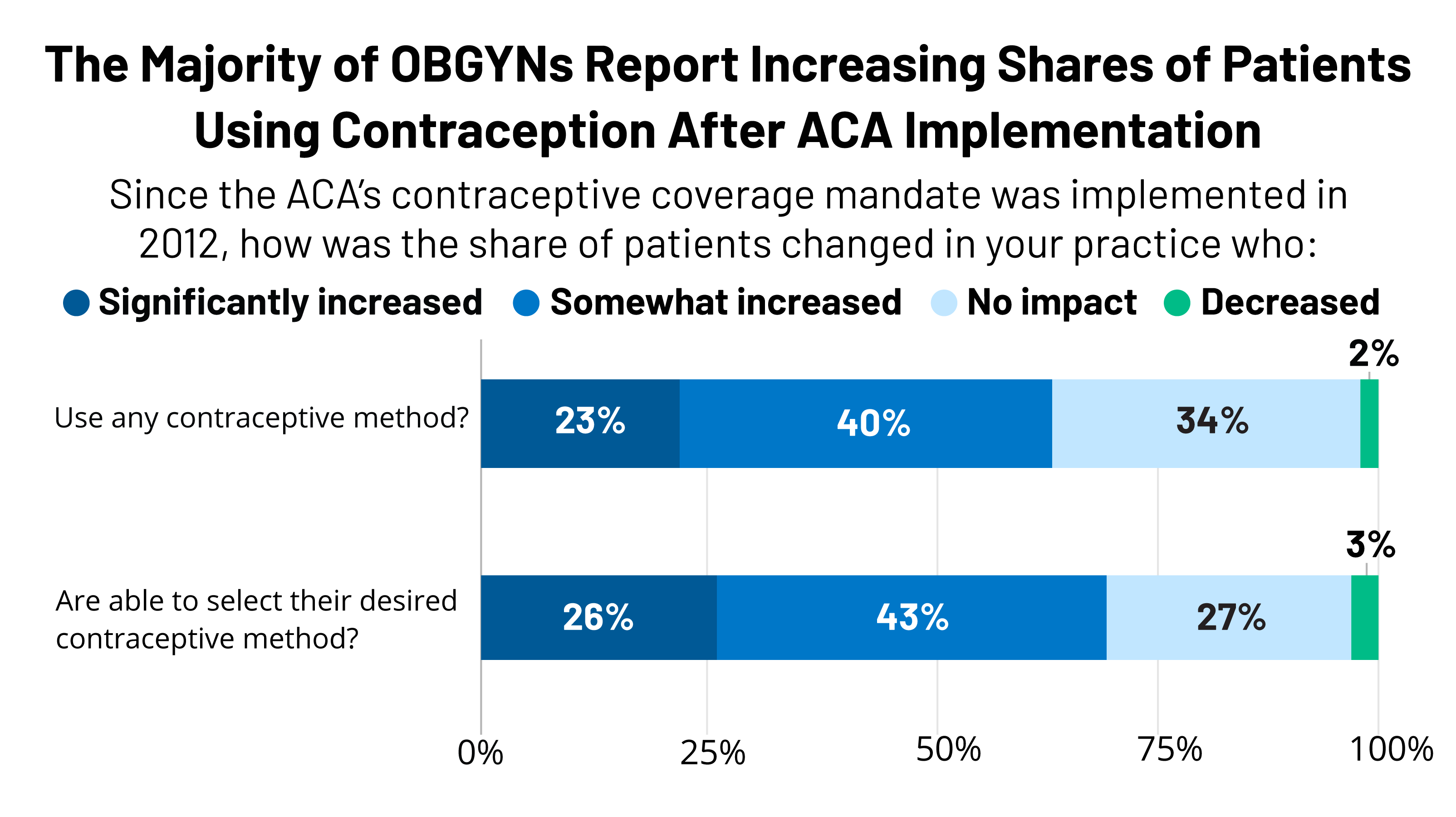
- Over six in ten OBGYNs reported an increase in the share of their patients who were using any contraceptive method (63%) as well as their desired contraceptive method (69%) since implementation of the ACA’s contraceptive coverage requirement in 2012.
- Over one in four (28%) reported that recent state-level abortion regulations including gestational age limits and regulations of providers have had a negative impact on their ability to provide quality reproductive health care; the majority (68%), however, reported that new abortion regulations have had no impact on care. Only 3% said that they improved care.
- When asked about career satisfaction, 70% of OBGYNs reported they would choose the same medical specialty, while a minority said they would choose a different specialty (19%) or not be a physician at all (10%).
Conclusions and Implications
Our findings suggest that patients may experience gaps in the availability of comprehensive SRH care provision depending on where they seek care and the providers they see. The vast majority of OBGYNs provided most forms of hormonal contraception, STI testing, cervical cancer screening, basic infertility diagnostics and prenatal care, but only a minority provided emergency contraception, abortion care, PrEP for HIV prevention, gender affirming care and resources to address psychosocial needs. This may reflect differences in training, personal preferences, and resource availability among OBGYNs.
Regional variation in SRH provision were was observed, particularly regarding the availability of same-day LARC insertions, abortion provision, and preparedness to meet the needs of LGBTQ patients. This could suggest that differences in state-level policies around SRH care, including the decision to expand Medicaid or not, may be influencing practice.
Variations in service provision were also observed by physician age. Younger physicians more often reported providing all methods of contraception, same-day LARCs, PrEP for HIV prevention, prenatal care and gender affirming care compared to the oldest group of OBGYNs.
Across several measures, a more comprehensive array of SRH services was available from OBGYNs who practiced in health centers/clinics rather than private office-based practices. While the reason for this difference is unknown based on this survey, it could perhaps reflect adherence to guidelines set out by the Health Resources & Services Administration’s Bureau of Primary Health Care Health Center Program and the Office of Population Affairs’ (OPA) Quality Family Planning Guidelines. It is notable that the vast majority of OBGYNs reported they accept Medicaid patients in their practice, and OBGYNs who served a large share of Medicaid patients had similar practice patterns compared to those who do not serve many Medicaid patients.
Most OBGYNs reported following reproductive health policy debates closely but had mixed perspectives on how health policy changes influenced their practices. For example, most OBGYNs perceived increases in the share of their patients using contraception since implementation of the ACA contraceptive coverage mandate, but a minority perceived any impact of recent abortion regulations on their ability to provide quality reproductive health care. This could be attributed to the sizable variation across the country in the adoption of abortion restrictions compared to the impact of the ACA’s contraceptive requirement that affected most women with private coverage regardless of their state of residence.
Overall, we observed heterogeneity in which SRH services OBGYNs provide, varying by both physician and practice characteristics. Gaps in SRH provision that have been highlighted from this survey warrant attention at the provider, institutional and policy level, in order to continue to strive for improved patient outcomes and experiences.
