By KIP SULLIVAN JD 
On the morning of December 21, I opened my copy of the New York Times to find an op-ed that said almost exactly what I had said in a two-part article The Health Care Blog posted two weeks earlier. The op-ed criticized the Hospital Readmissions Reduction Program (HRRP), one of dozens of “value-based payment” programs imposed on the Medicare fee-for-service program by the Affordable Care Act. The HRRP punishes hospitals if their rate of readmissions within 30 days following discharge exceeds the national average. The subtitle of the op-ed was, “A well-intentioned program created by the Affordable Care Act may have led to patient deaths.”
The first half of the op-ed made three points: (1) The HRRP appears to have reduced readmissions by raising the rate of observation stays and visits to emergency rooms; (2) the penalties imposed by the Centers for Medicare and Medicaid Services (CMS) for “excessive readmissions” have fallen disproportionately on “safety net hospitals with limited resources”; and (3) “there is growing evidence that … death rates may be rising.”
That’s exactly what I said in articles published here on December 6 and December 7. In Part I, I described the cavalier manner in which the Medicare Payment Advisory Committee (MedPAC) endorsed the HRRP in its June 2007 report to Congress. In Part II, I criticized the methodology MedPAC used to defend the HRRP in its June 2018 report to Congress, and I compared that report to an excellent study of the HRRP published in JAMA Cardiology by Ankur Gupta et al. which suggested the HRRP is raising mortality rates. In its June 2018 report, MedPAC had claimed the HRRP has reduced the rate at which patients targeted by the HRRP were readmitted within 30 days after discharge without increasing mortality. Gupta et al., on the other hand, found that for one group of targeted patients – those with congestive heart failure (CHF) – mortality went up as 30-day readmissions went down.
A second rigorous study contradicts MedPAC’s sloppy report
I was happy to see someone seemingly channeling me in the op-ed section of the New York Times. But, of course, they weren’t. After I got a third of the way through the op-ed, it became apparent the authors, Rishi Wadhera and two other cardiologists, were announcing the publication of a new study in the Journal of the American Medical Association that confirmed Gupta et al.’s findings, and added one more count to the indictment of the HRRP: The HRRP may be killing pneumonia patients as well. Wadhera et al. reported that the mortality rate within 30 days of discharge for both CHF and pneumonia patients rose in 2010, the year the HRRP was announced (that is, the year it was authorized by the ACA), and again in 2012, the year the HRRP was implemented. The three authors concluded with a question almost identical to the one I posed in my article: “Why are policies that profoundly influence patient care not rigorously studied before widespread rollout?”
In an interview, Dr. Robert Yeh, one of the three authors, was asked why their study’s conclusion differed from MedPAC’s. Dr. Yeh replied, “Because the methods employed in the MedPAC report are not clear to us at this time, I can’t really comment on why our results might differ.”
I was glad to hear that someone else found MedPAC’s report on the HRRP to be convoluted. The oddest feature of MedPAC’s methodology was its failure to break out inpatient mortality from post-discharge mortality. MedPAC lumped the two mortality rates into one rate, thus making it impossible for readers to assess what happened to mortality after discharge before and after the implementation of the HRRP. MedPAC’s rationale for this decision was that a slight increase in hospice use over their study period (2008 to 2016) might somehow distort the data.
Wadhera et al. not only declined to make that baffling mistake, they refined their post-discharge data even further: They examined 30-day mortality rates among patients who were readmitted within the 30-day window separately from mortality among those who were not. They found that the increase in mortality within the 30-day-post-discharge period was driven primarily by deaths among patients who were not readmitted within the 30-day window. The authors, and an accompanying editorial by Dr. Gregg Fonarow, noted that this evidence suggested causality – that the HRRP was killing CHF and pneumonia patients by encouraging hospitals to put off readmitting patients until after the 30-day post-discharge period. As Dr. Fonarow put it, “This finding, in particular, enhances the likelihood of a causal relationship between the HRRP … and the harm observed.” (p. 2540)
Wadhera et al. also examined the one excuse MedPAC offered for lumping inpatient mortality rates with post-discharge mortality rates, i.e., that the rate at which Medicare beneficiaries are being discharged to hospices rose over MedPAC’s study period (2008 to 2016), and somehow this would undermine the reliability of any findings. When Wadhera et al. removed patients discharged to a hospice from the 8 million patients in their sample, they got the same results. This is not surprising. The percent of patients discharged to hospices is small. Among CHF patients, for example, the discharge rate to hospices was just 5 percent in 2014, up from 2 percent in 2005.
Wadhera et al.’s methodology was superior to MedPAC’s in three other respects: Their sample size was larger (8 million versus 3 million); they created a pre-2010 baseline twice as long as the one MedPAC used (2006-2010 versus 2008-2010); and they used more accurate risk adjustment to reduce the probability that the health of the patients varied over the periods studied.
Toxic triage
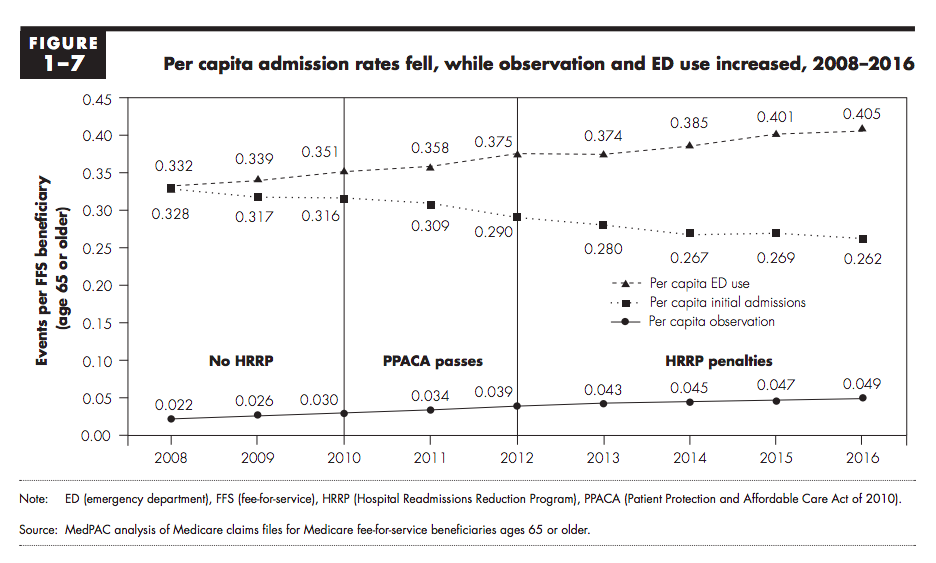
Most observers who examine the HRRP, including all of the authors I have mentioned here (Gupta et al., MedPAC, Wadhera et al., and Fonarow), comment on the startling increase in emergency department visits and use of observation stays since the early 2000s. This increase in ED visits and observation stays correlates strongly with the decrease in readmissions. We see this pattern among patients targeted by the HRRP, among Medicare beneficiaries generally, and among the non-elderly privately insured. [1] The figure below displays the pattern for Medicare beneficiaries between 2008 and 2016. ED use rose 22 percent and use of observation stays rose 123 percent between 2008 and 2016. These increases dwarfed the 20 percent per-beneficiary decline in readmissions over that period. The combined increase in ED and observation-stay use was five times the decline in readmissions. It is conceivable but unlikely, given the short time period graphed in the figure, that some of the increase in ED use is due to growing morbidity among people over 65. Gupta et al., who had access to medical records data (not just claims data), reported no increase in morbidity in CHF patients over the period 2006 to 2014.
The universality of this inverse correlation suggests the HRRP cannot be its sole cause. But the enormous disproportion in these trends is disturbing. It is a siren in the night warning us that hospitals are under great pressure not to admit patients within 30 days after discharge, and their reactions to that pressure are doing more harm than good. The reports by Gupta et al. and Wadhera et al. indicate that the substitution of ED visits and observation stays for readmissions, whatever its cause, is harming pneumonia and CHF patients.
Evidence-based medicine for thee, faith-based health policy for me
It is way past time for MedPAC, CMS and Congress to respond to the siren. They should start by shutting down the HRRP until that happy day when research demonstrates that punishing hospitals for readmissions, however defined, is a safe and effective method of cutting Medicare costs. They should also review the process by which MedPAC persuaded Congress to enact the HRRP in the first place (as I did in my December 6 article). MedPAC should lead this review because it was MedPAC, more than any other individual or agency, that persuaded Congress to create the HRRP. Such a review would serve the same function as an investigation by the National Transportation Safety Board of a plane crash – it would address the question, How did this happen and how do we prevent it from happening again?
An honest review would conclude that the single most important reason a risky program like the HRRP was thrust upon the nation’s elderly without pre-testing was the double standard that managed care advocates have promoted for the last half-century. According to this standard, it’s just fine for managed care advocates like MedPAC to lecture doctors and hospitals about practicing “evidence-based medicine,” but MedPAC et al. do not have to practice “evidence-based health policy.” They can promote policies on the basis of little or no evidence, and they can persist in doing so even after evidence piles up indicting their faith-based policies. An honest review would conclude that faith-based health policy is a form of malpractice and should be condemned. It would conclude that MedPAC must from now on recommend to Congress only those proposals which have been shown by rigorous testing to be safe and effective.
Footnotes:
[1] In my December 7 article, I cited a study by Sabbini and Wright that found that readmission rates as “readmission” is almost always defined – readmission within 30 days following discharge following an admission – have not fallen if we count readmissions that follow observation stays. The study, which focused on the privately insured, found that if observation stays were added to admissions, and if unplanned admissions after observation stays within 30 days were added to readmissions, the apparent decline in readmissions as traditionally defined disappeared. This pattern probably holds for Medicare beneficiaries as well. In fact, in view of the enormous increase in observation-stay use among Medicare beneficiaries (123 percent over the period 2008-2016) versus the modest decline in readmissions over that period (20 percent), we may predict that a similar study focused on Medicare beneficiaries would find a substantial increase in readmissions as Sabbini and Wright defined the term.
Kip Sullivan is a member of the Health Care for All MN advisory board, and of MN Physicians for a National Health Program.
